 How often does a patient come in your door that is in excellent health: eats healthy, exercises, no high blood pressure, no high cholesterol, no medications? Now, how often does a patient come in your door that is 20-30 pound overweight, on high blood pressure medications, on a statin for high cholesterol, pre-diabetic, and leads a fairly sedentary life other than “socializing”? I first became interested in diet and hearing while completing my Au.D. at Rush University. Around that time there was a critical mass of literature developing examining the relationship between diet and hearing. These studies consisted primarily of animal based work exploring influence of micronutrients with antioxidant mechanisms (e.g. vitamin A, C, E, and etc.) and other antioxidant compound
How often does a patient come in your door that is in excellent health: eats healthy, exercises, no high blood pressure, no high cholesterol, no medications? Now, how often does a patient come in your door that is 20-30 pound overweight, on high blood pressure medications, on a statin for high cholesterol, pre-diabetic, and leads a fairly sedentary life other than “socializing”? I first became interested in diet and hearing while completing my Au.D. at Rush University. Around that time there was a critical mass of literature developing examining the relationship between diet and hearing. These studies consisted primarily of animal based work exploring influence of micronutrients with antioxidant mechanisms (e.g. vitamin A, C, E, and etc.) and other antioxidant compound  found in diet usually in small amounts (e.g. alpha lipoic acid, resveratrol, cysteine (NAC), D-MET, and etc.). You can find a review in the July/Aug 2011 issue of Audiology Today. I found this all very intriguing, but there was very little evidence at this point that dietary intake could influence susceptibility to hearing loss in humans. Only a few case-control and prospective studies had been performed in humans. In these cases diet was either supplemented with a specific nutrient, e.g. folic acid (Durga et al., 2007) or a specific dietary component was manipulated, e.g. saturated fat (Rosen et al., 1970).
found in diet usually in small amounts (e.g. alpha lipoic acid, resveratrol, cysteine (NAC), D-MET, and etc.). You can find a review in the July/Aug 2011 issue of Audiology Today. I found this all very intriguing, but there was very little evidence at this point that dietary intake could influence susceptibility to hearing loss in humans. Only a few case-control and prospective studies had been performed in humans. In these cases diet was either supplemented with a specific nutrient, e.g. folic acid (Durga et al., 2007) or a specific dietary component was manipulated, e.g. saturated fat (Rosen et al., 1970).
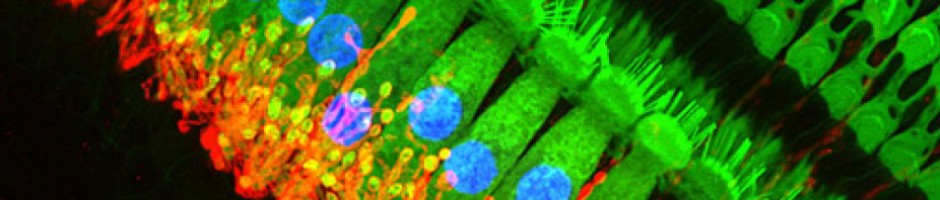
 When I started my Ph.D. at Vanderbilt, my mentor Linda Hood and I began discussing ways to look at diet and its influence on hearing in humans. My critique of the literature was that it was too focused on trying to find a “magic bullet”, the super-nutrient that would protect us all from age, noise, and ototoxic hearing loss. The first step was to begin an extensive literature review on anything diet and hearing and increase my personal knowledge through courses in nutrition, biochemistry, and molecular physiology. This led to epidemiological studies (Spankovich et al., 2011 and Gopinath et al, 2011) in collaboration with the Blue Mountains Hearing Study (a longitudinal study of hearing and contributing cofactors in Australia). These were some of the first large-scale epidemiological studies to examine the relationship between dietary intake and objective measures of hearing in humans. Interestingly, our results supported much of the animal-based work.
When I started my Ph.D. at Vanderbilt, my mentor Linda Hood and I began discussing ways to look at diet and its influence on hearing in humans. My critique of the literature was that it was too focused on trying to find a “magic bullet”, the super-nutrient that would protect us all from age, noise, and ototoxic hearing loss. The first step was to begin an extensive literature review on anything diet and hearing and increase my personal knowledge through courses in nutrition, biochemistry, and molecular physiology. This led to epidemiological studies (Spankovich et al., 2011 and Gopinath et al, 2011) in collaboration with the Blue Mountains Hearing Study (a longitudinal study of hearing and contributing cofactors in Australia). These were some of the first large-scale epidemiological studies to examine the relationship between dietary intake and objective measures of hearing in humans. Interestingly, our results supported much of the animal-based work.
 However, I recognized several limitations in our analysis (for more information see two-part 20Q series with Gus Mueller at AudiologyOnline entitled Healthy Eating Makes for Healthy Hearing: The Recipe and Today’s Special). We performed what is referred to as a single-nutrient analysis. The dietary data was collected by having people fill out a food frequency questionnaire (i.e., subject indicates what their average intake of different foods) then that is entered into a database to derive the estimated intake of every nutrient you can think of. Now foregoing problems with patient accuracy in self-reporting intake and cross-sectional nature of this design; the single nutrient analysis takes each individual nutrient and puts it into a statistical model (while adjusting for covariates) to determine if there is an association with our outcome measure (e.g. hearing thresholds, OAEs, etc.). The single-nutrient analysis has several limitations: 1) you end up performing a lot of analyses, which increases the likelihood of finding an association by chance; 2) nutrients have numerous known and unknown interactions both biochemically and statistically, not addressed with this model; 3) we do not eat single nutrients, we eat a diet.
However, I recognized several limitations in our analysis (for more information see two-part 20Q series with Gus Mueller at AudiologyOnline entitled Healthy Eating Makes for Healthy Hearing: The Recipe and Today’s Special). We performed what is referred to as a single-nutrient analysis. The dietary data was collected by having people fill out a food frequency questionnaire (i.e., subject indicates what their average intake of different foods) then that is entered into a database to derive the estimated intake of every nutrient you can think of. Now foregoing problems with patient accuracy in self-reporting intake and cross-sectional nature of this design; the single nutrient analysis takes each individual nutrient and puts it into a statistical model (while adjusting for covariates) to determine if there is an association with our outcome measure (e.g. hearing thresholds, OAEs, etc.). The single-nutrient analysis has several limitations: 1) you end up performing a lot of analyses, which increases the likelihood of finding an association by chance; 2) nutrients have numerous known and unknown interactions both biochemically and statistically, not addressed with this model; 3) we do not eat single nutrients, we eat a diet.
 Based on these self-critiques I began to explore other ways of looking at diet and hearing, which led to a recent analysis of dietary quality and hearing using the National Health and Examination Survey (NHANES) database. Rather than looking at single nutrients, Colleen Le Prell and I focused on a measure of dietary quality called the Healthy Eating Index, a measure of overall dietary quality based on 10 factors of dietary recommendations outlined by the U.S. Department of Agriculture (USDA). To make a long story short, the findings indicated that persons who ate a healthier dietary quality had better high frequency hearing thresholds that those that had poorer dietary quality in all age groups and in both sexes (see Spankovich & Le Prell 2013 for more information). Obviously our dietary quality is critical for our health in general, so it makes sense that hearing health may also be impacted.
Based on these self-critiques I began to explore other ways of looking at diet and hearing, which led to a recent analysis of dietary quality and hearing using the National Health and Examination Survey (NHANES) database. Rather than looking at single nutrients, Colleen Le Prell and I focused on a measure of dietary quality called the Healthy Eating Index, a measure of overall dietary quality based on 10 factors of dietary recommendations outlined by the U.S. Department of Agriculture (USDA). To make a long story short, the findings indicated that persons who ate a healthier dietary quality had better high frequency hearing thresholds that those that had poorer dietary quality in all age groups and in both sexes (see Spankovich & Le Prell 2013 for more information). Obviously our dietary quality is critical for our health in general, so it makes sense that hearing health may also be impacted.
Clinical Relevance
 The research that I briefly discuss above has a variety of goals. Numerous studies are focused on single or combinations of micronutrients or other antioxidant compounds to prevent acquired hearing loss; the idea of finding a specific nutrient or treatment that will serve as an otoprotecant that can be delivered as a supplement.
The research that I briefly discuss above has a variety of goals. Numerous studies are focused on single or combinations of micronutrients or other antioxidant compounds to prevent acquired hearing loss; the idea of finding a specific nutrient or treatment that will serve as an otoprotecant that can be delivered as a supplement.  Some of these are based on micronutrients we can obtain in our diet, while others are compounds based on chemicals derived through diet in trace levels. There are remaining questions in regards to the mechanism of these compounds as well as safety of long-term use. Some agents may be limited to acute application for acute exposures (e.g. while taking ototoxic drug); while others may have better profiles for long-term application (e.g. age). The other major avenue is not through a specific nutrient, but rather through good old-fashioned healthy living, i.e. eating right and exercise.
Some of these are based on micronutrients we can obtain in our diet, while others are compounds based on chemicals derived through diet in trace levels. There are remaining questions in regards to the mechanism of these compounds as well as safety of long-term use. Some agents may be limited to acute application for acute exposures (e.g. while taking ototoxic drug); while others may have better profiles for long-term application (e.g. age). The other major avenue is not through a specific nutrient, but rather through good old-fashioned healthy living, i.e. eating right and exercise.
 I often get asked what supplement or specific nutrients I would recommend for a patient. I first make the obvious statement, I am audiologist, I am not a nutritionist or something to that effect, and you should discuss any changes in your diet or exercise regimen with your physician or a nutrition expert. With that being said here is a list of some simple changes that will likely improve your and your patients overall health, lose a little weight, and maybe even reduce susceptibility to hearing loss. Recognize these are only general recommendation and do not apply to everyone; medications, age, pregnancy, disease can all impact what dietary needs are best for an individual.
I often get asked what supplement or specific nutrients I would recommend for a patient. I first make the obvious statement, I am audiologist, I am not a nutritionist or something to that effect, and you should discuss any changes in your diet or exercise regimen with your physician or a nutrition expert. With that being said here is a list of some simple changes that will likely improve your and your patients overall health, lose a little weight, and maybe even reduce susceptibility to hearing loss. Recognize these are only general recommendation and do not apply to everyone; medications, age, pregnancy, disease can all impact what dietary needs are best for an individual.
- Eat a balanced diet. There are a lot of “diets” out there, high-carb, low-carb, low-fat, high-protein, etc. But when I say balanced diet I am not referring to a weight loss plan,
 but a lifestyle plan. You can check out the USDA website for specific information. You need good sources of protein, carbohydrates and yes even fat in your diet. Overloading or under serving on one is not a good idea. For example, in longevity studies with animals, caloric intake can be manipulated (reduced by about 20-30%) and increase the lifespan of the animal. Turns out you can reduce fat = no effect, reduce carbs = no effect, but reducing protein = animals lives longer. Now it is not that protein is bad for you, protein is actually critical for good health and supply of essential amino acids, but too much may reduce lifespan.
but a lifestyle plan. You can check out the USDA website for specific information. You need good sources of protein, carbohydrates and yes even fat in your diet. Overloading or under serving on one is not a good idea. For example, in longevity studies with animals, caloric intake can be manipulated (reduced by about 20-30%) and increase the lifespan of the animal. Turns out you can reduce fat = no effect, reduce carbs = no effect, but reducing protein = animals lives longer. Now it is not that protein is bad for you, protein is actually critical for good health and supply of essential amino acids, but too much may reduce lifespan. - Eat This! Green leafy vegetables (e.g. kale, spinach, greens), onions,
 mushrooms, berries (e.g. blueberries, raspberries, strawberries), variety of colored vegetables (e.g. carrots, tomatoes (really a fruit), broccoli, artichoke, brussel sprouts, bell peppers, and etc.), nuts and seeds (e.g. almonds, sunflower seeds, not peanuts), other fruits and veggies (e.g. oranges, watermelon, bananas, apples, avocado, and etc.), the brown versions of the white foods to reduce (e.g. sweet potatoes instead of white, brown rice, and etc.) and fish that are lower in mercury.
mushrooms, berries (e.g. blueberries, raspberries, strawberries), variety of colored vegetables (e.g. carrots, tomatoes (really a fruit), broccoli, artichoke, brussel sprouts, bell peppers, and etc.), nuts and seeds (e.g. almonds, sunflower seeds, not peanuts), other fruits and veggies (e.g. oranges, watermelon, bananas, apples, avocado, and etc.), the brown versions of the white foods to reduce (e.g. sweet potatoes instead of white, brown rice, and etc.) and fish that are lower in mercury. - Not That! Processed foods (e.g. cold cuts, fast food, fried foods, frozen dinners, high
 fructose corn syrup, and etc.), these are high in sodium, sugars and processing can remove many important nutrients. Foods high in saturated and trans-fats (e.g. cheese, grain-fed red meat, fried foods, oils and etc.), however not all fat is bad (e.g. seeds, nuts, avocados, fish and etc [these are in the foods to increase above]). White foods (e.g. white potatoes, white rice, white flour, white bread, white sugar, white pasta); have high glycemic indexes which leads to inflammation, which leads to heart disease, diabetes, cancer, etc.
fructose corn syrup, and etc.), these are high in sodium, sugars and processing can remove many important nutrients. Foods high in saturated and trans-fats (e.g. cheese, grain-fed red meat, fried foods, oils and etc.), however not all fat is bad (e.g. seeds, nuts, avocados, fish and etc [these are in the foods to increase above]). White foods (e.g. white potatoes, white rice, white flour, white bread, white sugar, white pasta); have high glycemic indexes which leads to inflammation, which leads to heart disease, diabetes, cancer, etc. - Other recommendations. If you like red meat, that is ok, however it is preferable to
 eat grass-fed beef. Grass-fed beef has a more balanced ratio of omega fatty acids 3 and 6, where grain fed is 15-20 omega-6 to every 1 omega-3. Eggs are great, recent research really questions if cholesterol intake has any impact on heart disease, if you eat all the food recommended above and reduce the ones not recommended you will likely be getting plenty of good fat in your diet. Dairy products are a difficult topic. The hormones are to be avoided, but there are also benefits of vitamin D and calcium, you may be smart to try almond milk.
eat grass-fed beef. Grass-fed beef has a more balanced ratio of omega fatty acids 3 and 6, where grain fed is 15-20 omega-6 to every 1 omega-3. Eggs are great, recent research really questions if cholesterol intake has any impact on heart disease, if you eat all the food recommended above and reduce the ones not recommended you will likely be getting plenty of good fat in your diet. Dairy products are a difficult topic. The hormones are to be avoided, but there are also benefits of vitamin D and calcium, you may be smart to try almond milk.
 These recommendations are not a diet; eat all the spinach you want! They are a lifestyle change. Variety is important; you don’t have to eat the same thing every day. Also, it is ok to have that fast food once in a while, we are only human. The key really is balance. If you make the simple changes of reducing processed foods, cutting down on white foods, and eating more fresh vegetables and fruit, it will go a long way.
These recommendations are not a diet; eat all the spinach you want! They are a lifestyle change. Variety is important; you don’t have to eat the same thing every day. Also, it is ok to have that fast food once in a while, we are only human. The key really is balance. If you make the simple changes of reducing processed foods, cutting down on white foods, and eating more fresh vegetables and fruit, it will go a long way.
So what can I tell my patients? Well, you do not need to give them a specific diet. Simply recommend that they eat healthy and exercise and it may reduce susceptibility to further hearing loss. If they are interested in a specific diet then they should follow-up with a nutritionist who can work with them in developing a plan.
Summary
 What we eat influences our health; it makes sense that it may also impact our susceptibility to hearing loss. No supplement can replace a healthy diet, though they may be beneficial. The research on benefits of over the counter supplements for prevention of chronic disease is not that great, with some studies even suggesting increases in disease and mortality with use of multivitamin supplements. When it comes down to it, even with all the advances in technology and science, your mom was right “eat your vegetables and go outside and play”.
What we eat influences our health; it makes sense that it may also impact our susceptibility to hearing loss. No supplement can replace a healthy diet, though they may be beneficial. The research on benefits of over the counter supplements for prevention of chronic disease is not that great, with some studies even suggesting increases in disease and mortality with use of multivitamin supplements. When it comes down to it, even with all the advances in technology and science, your mom was right “eat your vegetables and go outside and play”.
 Christopher Spankovich is a Research Assistant Professor in the Department of Speech, Language, and Hearing Sciences at the University of Florida. His academic training includes a master of public health (M.P.H.) from Emory University, a clinical doctorate in audiology (Au.D.) from Rush University, and a research doctorate in hearing sciences (Ph.D.) from Vanderbilt University. His current research includes: dietary health and hearing, DPOAE fine structure and early identification, and novel methods of otoprotection. He recently was selected as a member of the 2012 AAA Jerger Future Leaders of Audiology Conference (JFLAC) cohort.
Christopher Spankovich is a Research Assistant Professor in the Department of Speech, Language, and Hearing Sciences at the University of Florida. His academic training includes a master of public health (M.P.H.) from Emory University, a clinical doctorate in audiology (Au.D.) from Rush University, and a research doctorate in hearing sciences (Ph.D.) from Vanderbilt University. His current research includes: dietary health and hearing, DPOAE fine structure and early identification, and novel methods of otoprotection. He recently was selected as a member of the 2012 AAA Jerger Future Leaders of Audiology Conference (JFLAC) cohort.
References:
Durga J, Verhoef P, Anteunis L, Schouten E, & Lok F. (2007). Effects of folic acid supplementation on hearing in older adults: a randomized, controlled trial. Ann Intern Med 14(6):1-9.
Gopinath B, Flood VM, Teber E, McMahon CM, et al. (2011). Dietary intake of cholesterol is positively associated and use of cholesterol-lowering medication is negatively associated with prevalent age-related hearing loss. Journal of Nutrition 141(7):1355-61
Rosen S, Olin P, & Rosen HV (1970). Dietary prevention of hearing loss. Acta Otolaryngol 70(4):242-247.
Spankovich C. (2011). Bench to Bedside: we “ear” what we eat. Aud Today 23(4):33-41.
Spankovich C, Hood LJ, Silver HJ, Lambert W, Flood VM, & Mithcell P (2011). Associations between diet and both high and low pure tone averages and transient evoked otoacoustic emissions in an older adult population-based study. J Am Acad Audiol 22(1):49-58.
Spankovich C, & Le Prell CG. (2013). Healthy diets, healthy hearing: National health and nutrition examination survey, 1992-2002. Inter J of Aud 52:369-376.
Nice to see blog which may help to me. I have curiosity mind to know, do you have plan to write skin disorders please?
what specific information are you looking for? Let me know and I will see if I can help
I’m so glad you’re doing this research! You mentioned an uncertainty regarding dairy. Have you looked at raw milk? Others report a big difference in the health benefits of raw vs. pasteurized milk.
amanda:
thanks so much for following/reading this blog post by Dr. Spankovich; I will make sure he is aware of your question and either have him answer or answer on his behalf. On a separate note, I am personally intrigued by nutrition and its influence on various aspects of health; I had a family member who experienced dizziness, unilaterial HF SNHL, and tinnitus and to make a long story short, at the end of the day, after obvious things were ruled out, turned out his symptoms were related to a gluten allergy. From my own personal perspective, although not hearing related, I experienced significant health benefits when I moved to a Whole30 program. If interested, you can read about it at my personal blog called AU’s Adventures. Here is the link to the specific program I experienced (read from the bottom up as the most recent posts appear first so if you want background info, you gotta scroll down and read up). http://auadventures.wordpress.com/category/whole30-adventure/ It was a fascinating journey that makes me appreciate this guest blog post by Christopher that much more meaningful.
Sorry for the delayed response. I do not have a great deal of knowledge regarding benefits of raw vs pasteurized milk. There are many proponents of the health benefits of raw milk, however I think it is highly dependent on a reputable source. However, there are some “experts” like Joel Furhman, who suggest all dairy products should be avoided and are not meant for human consumption.